#1 HOSPITAL — AUSTRALIAN CAPITAL TERRITORY
- Wrong site surgery
Woman had surgery on wrong hip. “Catastrophic incident” hospital classed it as but only after woman asked why the wound dressings were on the wrong side. Hospital apologised to patient’s family but not to patient. The patient then had the operation on the correct side. The patient later died. Surgeon botched the 2nd hip operation but not the wrong 1st hip operation — strange that the surgeon hadn’t noticed the 1st operation on good hip had nothing wrong with it. Peculiarly, the ACT Health director-general then assured Canberrans that the health system was safe. Not for this patient.
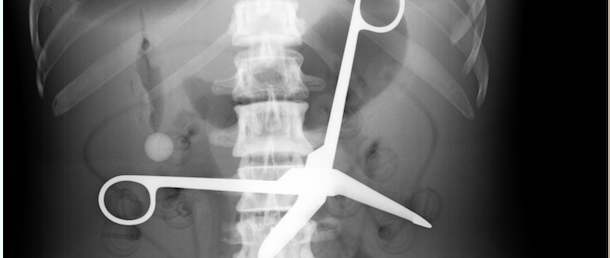
#2 HOSPITAL — NEW SOUTH WALES
- Equipment count-back failure
Woman admitted to hospital for bowel polyp removal. Endures sharp, cutting pain in her stomach for 18 months. Was told it was after-effects of surgery. Had colonoscopy, which revealed nothing. No doctor suggested she have an x-ray. When patient insists on an x-ray, revealed is a pair of 15cm surgical scissors, slightly open, lodged between her lower bowel and spine. The hospital said it did not count scissors after surgery because they were considered too large to lose.
#3 HOSPITAL — NORTHERN TERRITORY
- Overdose – failure to document meds dispensed
Woman attended hospital in the Red Centre for a scheduled caesarean but died after giving birth to daughter. Coroner found a communication breakdown between doctors and the patient was given an overdose of drug Prostaglandin. The high dosage brought on cardiac arrest at a time when the patient’s system was already compromised because of massive blood loss. There was no discussion between doctors about the dosage and, within minutes of being given it, her blood pressure rose so significantly that she was unable to recover. The mistaken dosage was a serious oversight, said the ACT coroner. Death is more than a serious oversight.
#4 HOSPITAL — QUEENSLAND
- Diagnosis failure
Young man attended cardiology clinic for 18 months for fast heart rate, shortness of breath, lethargy. Told to lose weight, get fit and sent him to rheumatologist. Doctor deemed cause was from too much Pepsi and takes him off all medication. Week later has chest pain, sees GP, told it’s indigestion, goes home and 2 hours later dies. Hospital treats his grieving family with disdain. Vehemently refused to answer family’s questions or provide medical records aggravating family further. Family alerts the Coroner. Inquest finds patient had cardiac problems and hospital had not ever conducted any cardiac investigations.
#5 HOSPITAL — SOUTH AUSTRALIA
- Intern training failure
Young woman attends hospital Emergency Department with profuse sweating and fever symptoms. Told she has over-exerted herself playing hockey and caught a chill. Intern fails to call another doctor, let alone a specialist for another opinion, and sends patient home with Panadol. Next day patient found dead. Autopsy revealed patient had cardiomyopathy.
#6 HOSPITAL — TASMANIA
- Blame shifting — doctor erred, nurse blamed
Man admitted to hospital for hip replacement. Surgery went OK but next day he couldn’t be resuscitated and dies. Doctor said due to natural causes. A pre-operative dose of anti-coagulants had been given to patient at home, but the intra-operative dose and subsequent doses had been omitted in hospital. Surgeon blamed nurse. Medical records reveal no doctor prescribed anti-coagulants following surgery. Autopsy found patient died of post-operative clot and noted resuscitation attempts had been conducted for 20 minutes.
#7 HOSPITAL — VICTORIA
- Wrong patient – name cross-check failure
Two women attended same clinic and saw the same doctor, the same day. Both women had same Christian names. Both needed breast biopsies which were done same date, same hospital by same doctor. One had breast cancer. One did not. 9 months later it was discovered the results had been muddled up. The patient with cancer is dead. The patient without cancer is alive but is minus a breast, had months of chemotherapy and an upper arm so large it will not fit into a regular-size sleeve.
#8 HOSPITAL — WESTERN AUSTRALIA
- Infection control failure
Man admitted to hospital for total knee replacement. Acquires post-operative staph infection. More surgery to washout knee infection. Then more surgery to re-do knee replacement. Acquires another post-operative infection requiring more surgery to wash out knee. Drug Chart disappears from patient’s medical record. Then knee replacement removed altogether and knee fused straight. 10-day hospital stay became 16 weeks. Man left a cripple with knee full of concrete.